Issue #1 - July 2024
Welcome to the very first issue of Craftsmanship!
This is a new beginning for me. I am very excited to put this all together to deliver a product and a platform dedicated to education and mastery in clinical dentistry.
In case this is the first time you are reading my work, my name is Omar and I am a dental student entering my final year of dental school. I know this journey towards mastering clinical dentistry will be years or even decades in the making but I am excited to share what I learn and document the process!
I will be sharing my experiences and reflections from dental school, evidence-based articles or literature reviews, clinical case spotlights written by guest clinicians, as well as any other interesting insights, quotes, book recommendations, you name it! Tangential to this newsletter I am also the host of the Craftsmanship Podcast, where I will delve into these ideas and much more in greater detail, bringing on guest clinicians for interviews, and case discussions, as well as solo episodes where I delve deep into dental topics, my experiences in dental school, and more! The link to the very first episode is right here:
🔍Clinical Case Spotlight
This month’s clinical case is presented by this month’s guest writer, Dr Ahmed Alkhaledi (Instagram @dentist_on_hand), a general dentist working in Ireland, whom I had the pleasure of meeting at a conference last year! He shares a case referred to him for a second opinion, where he saves a badly broken down, yet vital UR4, for a patient who was told that an extraction may be the only option! He explains his protocols for restoring this tooth while maintaining tooth vitality!
Presentation
The patient initially presented with solely the complaint of a ‘chipped’ tooth, there was no pain associated with the damage.
Assessment
This is arguably the most important step in restoring any tooth, an accurate assessment will greatly increase the efficiency of your workflow, allowing you to reliably plan a course of action, minimising the risk of running into difficulties intra-operatively.
For this specific case and for the vast majority of my ‘Heavily damaged’ teeth, the assessment revolves around 3 main tests, the first of which is the clinical presentation. It is important to assess the tooth intra-orally for any lesions/cracks/probings that may affect prognosis and/or possible treatment modalities. Following the clinical exam, a cold sensibility test is indicated. Even though root canal treatment can be carried out after restoration, this is not the ideal situation as it can be inefficient. Therefore, it is highly favourable to be aware of the endodontic status of a tooth before commencing any treatment.
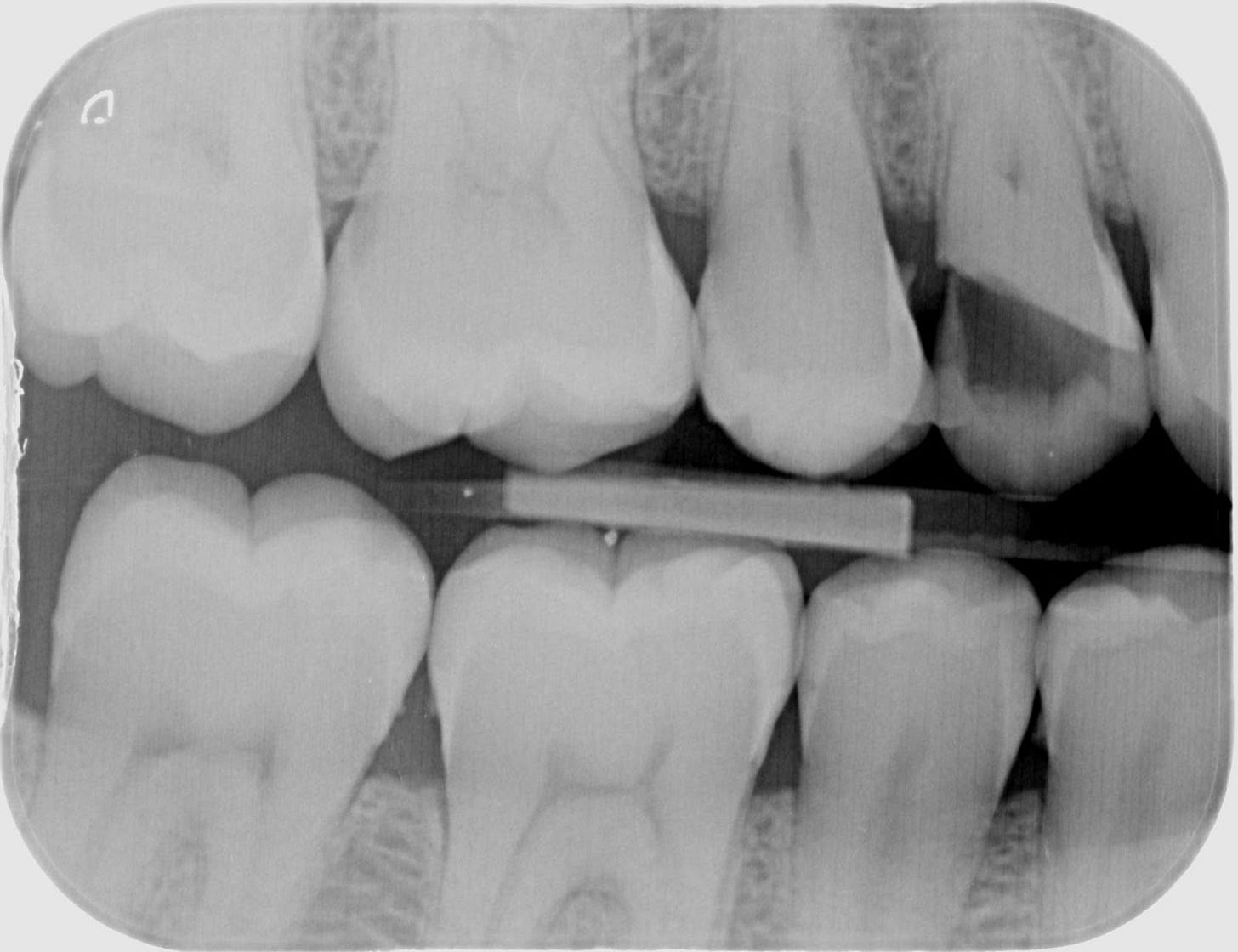
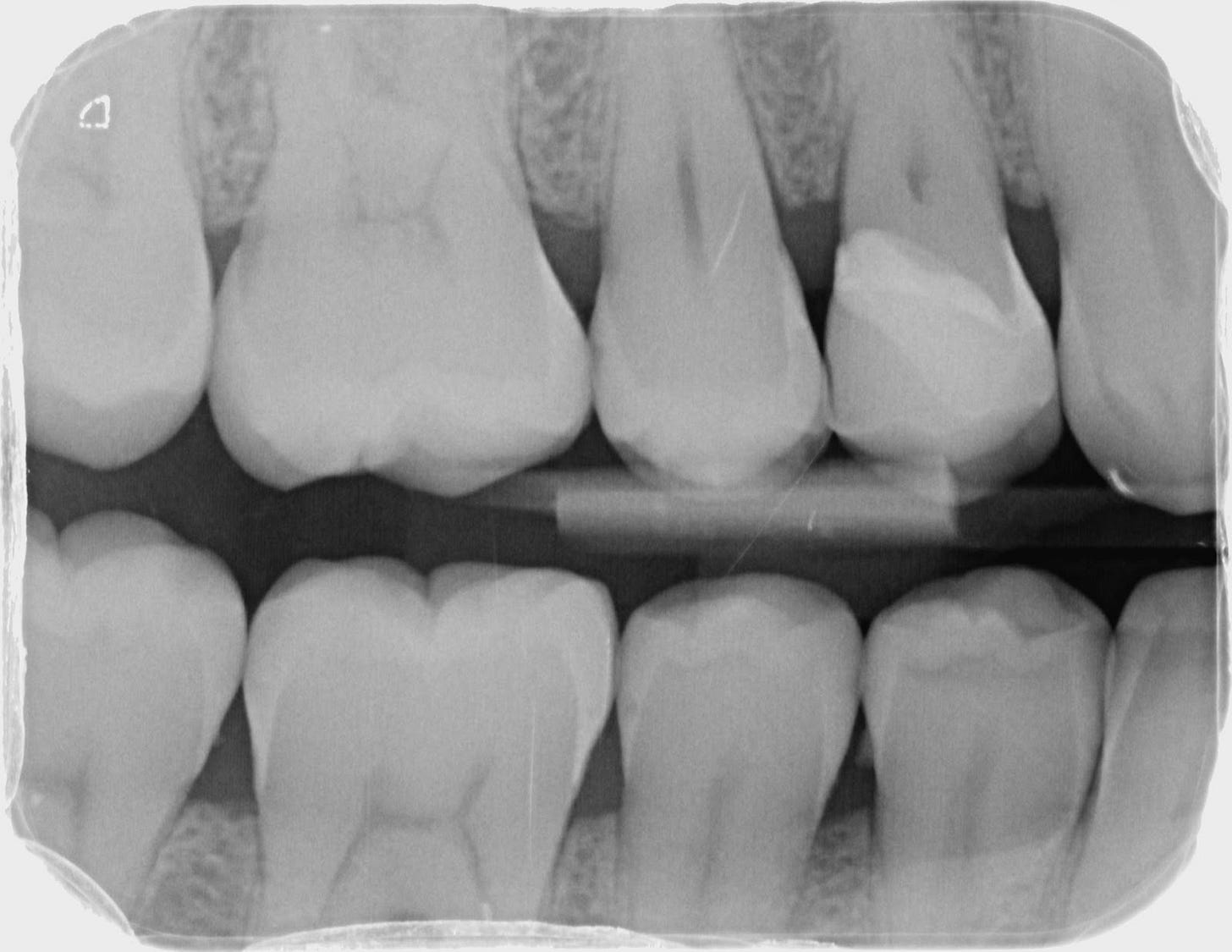
Radiographic imaging would be the next important examination to carry out, even though a PA may be required if an RCT is planned, a Bitewing radiograph is the only reliable way to assess both the presence of caries and its extent, mainly towards the bone.
The target tooth had no irregular probings, a fully normal response to cold, and a restorable margin.
Treatment - The Workflow
Given the extent of damage to the tooth and the presence of deep decay, a selective caries removal protocol followed by a deep margin elevation and indirect restoration was the chosen treatment plan, a minimally invasive option with hopes of preserving tooth tissue and pulp vitality.








Reflections
Whereas conventional dentistry would have you carry out crown lengthening +/- root canal therapy followed by a crown, with the help of good bonding protocols, a lot of teeth can be saved, and pulps kept alive without the need for any such destructive treatments. With that said, a DME is an extremely technique-sensitive procedure, and one that is heavily reliant on a multitude of factors, clinical skills, material choice, and time to name a few, and although it can do wonders in aiding the restoration of heavily damaged teeth, a sub-optimal DME can have dire consequences to the teeth and the associated periodontal tissues.
🦷Restorability & Direct vs. Indirect Restorations
This is the age-old question for restoring the badly broken down tooth, and with so many treatment options to choose from, it can be difficult to even know what to recommend to patients, let alone what to ultimately decide to move forward with. In this article, I aim to outline some of the main factors to consider when weighing up decisions like this one, to give more clarity as to how a dentist (or dental student!) can approach this scenario.
What I have recently learned on clinics is that the most important thing we can do as a dentist is solve the patient’s complaint. Every option should be considered through that lens, and we may find that this will eliminate several options that are otherwise clinically feasible.
After scouring PubMed in research for this article, I realised that if done to high quality, there is largely no significant difference between materials or digital/analogue techniques, and there is not sufficient, high-quality, and unbiased evidence supporting one approach over all the others.
In a systematic review looking at thirteen studies where direct and indirect composites were compared, the lowest-bias study found that there was no significant difference in the success rate, and the results with a higher risk of bias were also inconclusive. (Azeem and Sureshbabu) It is important to note the main influencing factor that was concluded was the amount of remaining tooth tissue, which is something I am sure you would have expected. This seems very intuitive, as we were all taught in dental school, that obtaining that 2mm ferrule circumferentially around a tooth is key to a good restorative prognosis, and several papers address factors like structural integrity, periodontal and endodontic status, which is really well summarised in this table:
(Dawood and Patel)
To delve deeper into these concepts, the first of which is the tooth’s structural integrity. Note that structural integrity here is most important for restorations that rely (at least partially) on mechanical retention. Purely adhesive restorations, such as the more modern, biomimetic adhesive onlays rely primarily on chemical adhesion, but may still incorporate some structural features that aid in retention and resistance. The features that can contribute to this may be unique depending on the scenario, but every tooth being restored will require adequate retention and resistance form, and the product of these gives the tooth good structural integrity. Retention form is of course the product of the features of a tooth that prevent the movement of a restoration along the path of insertion (generally axially), while resistance form is comprised of the features preventing movement of a restoration in the non-axial direction, such as rotational movements. For traditional full-coverage crowns, retention form can be made up of the clinical crown height and the taper of the preparation, while resistance form will come from preparations being shaped similar to the natural tooth, rather than circular and conical, and in some cases, slots and grooves can aid in resistance. Furthermore, key aspects of a tooth’s structural integrity include the potential need for a post and core system to be used to create this retention and resistance, as well as the 1.5-2mm (ideally) circumferential ferrule (Juloski et al.), whose primary role is to improve fracture resistance of the tooth.
The other aspects of the Restorability Index include the periodontal and endodontic status of the tooth in question, with periodontal status being important, as the periodontium forms the foundations for any tooth, and this should be stable ideally, but even in cases of minimal pocketing, restorability is not greatly affected. This becomes an issue when there is grade 2-3 furcation involvements, pockets greater than 5.5mm, and other signs like mobility. The endodontic status of the tooth is also crucial, as it is widely known that non-vital, endodontically-treated teeth are more brittle and prone to fracture. This however, does not directly affect restorability of the tooth as much as the complexity of the root canal system and endodontic disease, as well as the subsequent quality of any endodontic treatment done. The fact that a tooth is non-vital alone may not be the deciding factor when determining restorability; unless it is untreatable endodontically for whatever reason. It is cases where the periodontal to endodontic prognosis is very questionable that may need referral, or at least a multidisciplinary approach to improve the periodontal/endodontic condition, before definitively restoring the tooth.
Along with these more concrete, scientific factors determining the restorability and consequent options for treating a tooth, there are other, “human” factors that are key to determining whether direct or indirect restorations can be feasible. These can include finances, but also consider what phase of treatment is the patient in (they may not be prepared for indirect restorations that demand a higher level of oral hygiene), or whether there is adequate access and ability to isolate with rubber dam, which may be critical for direct composite restorations or indirect restorations whose cements rely primarily on chemical adhesion rather than traditional luting cements. From my perspective, it is crucial that treatment should only be done if these surrounding “human factors” can be met, such as the isolation during treatment and the oral hygiene for long-term maintenance.
I hope this serves as a brief overview of assessing restorability! This is the first article I am writing on this topic, so let me know what you think or if there are any other considerations! I have also listed my references below if you would like to delve deeper into this!
Referencing
Azeem, Rubeena Abdul, and Nivedhitha Malli Sureshbabu. “Clinical Performance of Direct versus Indirect Composite Restorations in Posterior Teeth: A Systematic Review.” Journal of Conservative Dentistry : JCD, vol. 21, no. 1, 2018, pp. 2–9, www.ncbi.nlm.nih.gov/pmc/articles/PMC5852929/, https://doi.org/10.4103/JCD.JCD_213_16.
Aziz, Ahmed, and Omar El-Mowafy. “Six-Year Clinical Performance of Lithium Disilicate Glass-Ceramic CAD-CAM versus Metal-Ceramic Crowns.” The Journal of Advanced Prosthodontics, vol. 15, no. 1, 1 Jan. 2023, pp. 44–44, https://doi.org/10.4047/jap.2023.15.1.44. Accessed 14 Aug. 2023.
Belli, Renan, et al. “Mechanical Fatigue Degradation of Ceramics versus Resin Composites for Dental Restorations.” Dental Materials, vol. 30, no. 4, Apr. 2014, pp. 424–432, https://doi.org/10.1016/j.dental.2014.01.003.
Dawood, A., and S. Patel. “The Dental Practicality Index – Assessing the Restorability of Teeth.” BDJ, vol. 222, no. 10, 26 May 2017, pp. 755–758, https://doi.org/10.1038/sj.bdj.2017.447.
Holme, William. “Gold versus Ceramic - Which Will Last Longer for Posterior Indirect Restorations?” Evidence-Based Dentistry, vol. 23, no. 4, 16 Dec. 2022, pp. 166–167, https://doi.org/10.1038/s41432-022-0837-7.
Juloski, Jelena, et al. “Ferrule Effect: A Literature Review.” Journal of Endodontics, vol. 38, no. 1, 2012, pp. 11–9, www.ncbi.nlm.nih.gov/pubmed/22152612, https://doi.org/10.1016/j.joen.2011.09.024.
Rocha Gomes Torres, Carlos, et al. “Computer‐Aided Design and Computer‐Aided Manufacturing Indirect versus Direct Composite Restorations: A Randomized Clinical Trial.” Journal of Esthetic and Restorative Dentistry, 29 Sept. 2021, https://doi.org/10.1111/jerd.12820. Accessed 30 Mar. 2022.
📒The Dental Journal
In this segment, I will delve into an experience or two from dental school, and share my reflections!
Over the past month, I have started my final year clinical schedule and this has been a huge step up from my previous experiences, as we have begun our outreach clinic placements. These placements are opportunities for us to develop our skills in a different environment, and so far my experience there has been more independent than that in my other clinics, which I enjoy. This did lead to me miscommunicating with my tutor on my regular patient clinics though, as I had become more accustomed to the more hands-off approach to outreach. If you don’t want to make the same mistake I did, consider establishing the level of communication that is expected of you by each clinical tutor you may have, as it will differ. This is very important because it ensures that everyone on the dental team is on the same page, and this will always be in the patient’s best interest.
Speaking of outreach clinics, I have found that I have spent most of my patient appointments making dentures at these clinics, and one aspect that has helped me with my prosthodontic work is to have a good understanding of the knowledge base firstly, to be able to bring that into my appointments, but also to have a systematic plan for carrying out the treatment. For example, when doing a jaw registration for a complete denture, or non-ICP case, ensure that you know what to check and when for both the upper and lower arches. For example, a great approach I learned from a mentor is to think of the upper arch for aesthetics, and the lower for function, so the checks and measurements you take should be based on that. This means that when recording the correct OVD, ensuring the upper rim is adjusted first to have the correct level of incisal show, and then having the lower denture be adjusted to create the desired OVD, would mean that both the function and aesthetics are achieved. This would not be the case if you remove wax from both rims when reaching that OVD, as the maxillary teeth may become too short aesthetically.
This Month’s Favourites
📚Book: Feel-Good Productivity by Ali Abdaal
I have been picking this book up quite regularly again to read an idea or two and I really believe this one strikes the perfect balance of aiming high and striving for excellence, while also ensuring the journey to get there is an enjoyable one. Having unbreakable discipline is priceless, but no one beats the person having fun while he is doing it, and that is what this book speaks about. Highly recommend this one!
💬Quote: By Don Simpson (a film producer)
The great thing about being 90% finished, is at least you know you're halfway there.
This quote highlights the difference between good work and great work, and that it takes an average amount of time and effort to produce something good, but disproportionately more time to produce something undeniable! As great as the minimalistic approach, and the 80/20 rule are, reaching the summit of the mountain can take twice the amount of effort it took to get most of the way up!
This brings us to the end of this very first issue of The Craftsmanship Newsletter! I hope you found this insightful and inspiring! If you are a dentist interested in writing for the newsletter, then don’t hesitate to contact me via Instagram @omar_dental_ !
If you enjoyed this issue, stay tuned for the next one, as well as The Craftsmanship Podcast on Spotify, and let me know if you have any suggestions!
Get Better Today!





